Many parents put their children to bed with a bottle of milk or juice. It seems like a harmless act, which helps the child settle down and get to sleep. While the parents have good intentions, they are unknowingly rotting their children’s teeth one nap at a time. Many children get into the habit of going down for a nap with a bottle. Most times, the parent’s are not willing to break the child of the habit as it will cause the child to cry and fuss until the habit is broken.
What is baby bottle tooth decay?
Baby bottle tooth decay affects children who drink bottles. It is a result of the baby taking a bottle when they are in bed. In this instance, the juice or milk lays on the baby’s teeth, and the resulting lactic acid causes cavities. The condition is not due to the child lying down, but rather because the milk and juice pool in the baby’s mouth because the child falls asleep before the liquid is swallowed. The upper front teeth are most affected by baby bottle tooth decay. This condition affects 18% of children in this age group.
Approximately 10% of children under the age of 5 have early childhood cavities that are caused by baby bottle tooth decay. Treating childhood cavities many times requires major dental work that can include oral surgery and extraction. The costs can be upwards of $5,000 to have the work performed.
Preventing bottle tooth decay
Baby bottle tooth decay is easy to prevent. First, do not offer the baby a bottle for a nap or at bedtime. If your child has already formed a habit of going down with a bottle, give them plain unsweetened water. Many times it is the baby bottle that the child is attached to, not the liquid inside it. Another tactic is to wean the baby from the bottle by one year old. You can do this by watering down the milk or juice until it is no longer wanted by the child. At the same time, begin to introduce sippy cups as a substitute during waking hours.
Fluoride treatments also substantially reduce early childhood tooth decay when combined with a good oral health regimen. A study by the University of Southern California concluded that children who did not undergo fluoride treatments were 2.5 times at greater risk for developing tooth decay.
Long term affects of baby bottle tooth decay
Studies indicate that early tooth decay has long term affects, as it opens the door for future tooth decay. Children under 5 who experience tooth decay are at greater risk for tooth decay than those who do not have tooth decay during the first 5 years of life. The American Dental Association goes as far to say that a history of cavities in the baby teeth is a conclusive predictor of future cavities. Early childhood tooth decay can cause poor eating habits, speech problems, low self-esteem, delayed growth, and social problems.
Does breast milk cause tooth decay?
The answer is no. Many assume that breast milk will have the same effect on a child’s teeth as cow milk, particularly breastfeeding while lying down at night. This is not the case as there has not been a link established between the two. Extensive research has been conducted on human skulls between 500-1000 years old, before baby bottles were used. These children were obviously breastfed. The research indicated that the children did not have the type of tooth decay associated with baby bottle tooth decay.
One of the reasons cited for why breastfeeding does not mimic baby bottle tooth decay is because the breast milk does not pool in the baby’s mouth the same way that bottled milk does. The reason is that unlike a bottle, when the child stops suckling, the breast does not flow milk. In addition, the breast milk flows directly into the back of the child’s mouth, behind the teeth. As a breastfeeding baby sucks, he is swallowing at the same time.
Another study was done which examined the effects of lactose, found in milk, versus breastmilk. Breastmilk contains lactoferrin, which kills the bacteria that causes tooth decay (aka: strep mutans). In a 1999 issue of Pediatric Dentistry, it was concluded that if a child were exclusively fed breastmilk, he would not have pediatric tooth decay, unless they are genetically predisposed. Furthermore, breastmilk has a similar chemical effect on the child’s mouth as water.
Baby bottle tooth decay is preventable and failure to do so will cause long term affects upon your child’s future dental health overall. To ensure that your baby does not have baby bottle tooth decay schedule a checkup with your dentist at one year of age. If your child does have baby bottle tooth decay, it is treatable. If you have any concerns about your child’s teeth talk them over with your dentist at you next c
Wednesday, December 11, 2013
Tuesday, July 9, 2013
Ice Cream and Your Sensitive Teeth
It is summertime and
that means lots of ice cream! Well maybe for everyone else, but not for you
because you have sensitive teeth. Some people have sensitivity to hot drinks as
well. While an occasional pain is common, ongoing sensitivity to heat and cold
indicates that you have sensitive teeth. Millions of people suffer with the
pain of sensitive teeth. In many instances, the pain and discomfort cause
people to avoid their favorite foods. Some people‘s teeth are so sensitive that
cold air produces pain! What many people are not aware of is the fact that
sensitive teeth are easily treated and the effects are long lasting and, in some
instances, permanent.
What causes tooth sensitivity?
Tooth sensitivity occurs when the roots of the teeth are exposed by receding gums. The gums insulate the tooth’s roots and when they recede heat and cold penetrate the area. The roots contain tubules, which act like small pores, and lead directly to the nerve. The pain travels down the tubules when the heat and cold are present.
There are two reasons that gums recede. Improper brushing is the first reason. The American Dental Association estimates that about 60% of the population applies too much pressure when they brush their teeth. Over time, this added pressure causes the gum tissue to deteriorate and expose the roots. The second thing that causes the gums to recede is poor oral hygiene. Not brushing and flossing leads to plaque build up. The plaque hardens into tartar, which develops bacteria. The bacteria cause gingivitis that result in receded gums.
Another cause of sensitive teeth is worn down enamel. Usually, your saliva places calcium on the tooth’s enamel. The calcium provides a protective layer over the tubule’s openings. That protective layer is worn down for a variety of reasons. Tooth grinding and acidic foods can erode the enamel, as well as lead to receding gums. One of the most common causes is brushing your teeth excessively, especially with over the counter tooth polishes that are abrasive. When the protective layer is worn down, the tubules that lead to the nerve are exposed. When you eat ice cream, the cold fluid is forced into the tubules and it hits the nerve, causing pain. Sometimes even moderately cold or warm food and beverages will cause discomfort as well.
Preventing Sensitive Teeth
Sensitive teeth can be prevented by keeping the gums healthy. The first step to keeping the gums from receding is to reduce the pressure on your teeth when brushing. Since you have likely been brushing your teeth the same way for many years, brushing too hard can be a tough habit to break. Dentists advise using a motorized toothbrush. Electric toothbrushes will not work if too much pressure is applied, so using them helps reduce the wear and tear on the gums. Electric toothbrushes can be purchased for as little as $15 at the drugstore.
Proper oral hygiene is another way to prevent sensitive teeth. Most people only spend less than 45 seconds brushing their teeth, when in actuality it takes 2-3 minutes to thoroughly brush your teeth. Brushing your teeth quickly leaves some of the tooth structure unclean, which leads to plaque, then bacteria and ultimately gingivitis and receding gums.
Treating Sensitive Teeth
If you already have sensitive teeth, there is a treatment available. Potassium nitrate, which is found in sensitivity toothpastes, reduces tooth sensitivity. Sensodyne toothpaste is the #1 recommended toothpaste by dentists to treat sensitive teeth. Sensodyne is so effective that it begins to reduce tooth sensitivity within a few uses. When using Sensodyne, make sure that you are brushing properly and avoiding acidic foods to maximize its effectiveness.
When to see your dentist
If your sensitivity is so severe that switching to an electric brush and using sensitivity toothpaste does not work, then there is a treatment option available from your dentist. Your dentist can use oxalate compounds to treat the root, which will eliminate the sensitivity. There is also a bonding process available to seal the pores of the root.
If you have mild tooth sensitivity, there are toothpastes that are designed to protect the tubules. While it is an over the counter treatment, you should see your dentist to be sure that this is the right treatment. If the sensitivity is caused by another condition, your dentist can make a determination in one visit. In addition to the pain that tooth sensitivity causes, you can also develop inflammation that is not reversible. This condition can lead to an abscess that is only treated by oral surgery. Therefore, while tooth sensitivity starts out as a seemingly simple issue, it can lead to a serious condition. Your biannual checkups are the best time to discuss tooth sensitivity with your dentist. Your dentist can track the condition and visually inspect your teeth, which enables him to make the proper recommendations for your mouth.
What causes tooth sensitivity?
Tooth sensitivity occurs when the roots of the teeth are exposed by receding gums. The gums insulate the tooth’s roots and when they recede heat and cold penetrate the area. The roots contain tubules, which act like small pores, and lead directly to the nerve. The pain travels down the tubules when the heat and cold are present.
There are two reasons that gums recede. Improper brushing is the first reason. The American Dental Association estimates that about 60% of the population applies too much pressure when they brush their teeth. Over time, this added pressure causes the gum tissue to deteriorate and expose the roots. The second thing that causes the gums to recede is poor oral hygiene. Not brushing and flossing leads to plaque build up. The plaque hardens into tartar, which develops bacteria. The bacteria cause gingivitis that result in receded gums.
Another cause of sensitive teeth is worn down enamel. Usually, your saliva places calcium on the tooth’s enamel. The calcium provides a protective layer over the tubule’s openings. That protective layer is worn down for a variety of reasons. Tooth grinding and acidic foods can erode the enamel, as well as lead to receding gums. One of the most common causes is brushing your teeth excessively, especially with over the counter tooth polishes that are abrasive. When the protective layer is worn down, the tubules that lead to the nerve are exposed. When you eat ice cream, the cold fluid is forced into the tubules and it hits the nerve, causing pain. Sometimes even moderately cold or warm food and beverages will cause discomfort as well.
Preventing Sensitive Teeth
Sensitive teeth can be prevented by keeping the gums healthy. The first step to keeping the gums from receding is to reduce the pressure on your teeth when brushing. Since you have likely been brushing your teeth the same way for many years, brushing too hard can be a tough habit to break. Dentists advise using a motorized toothbrush. Electric toothbrushes will not work if too much pressure is applied, so using them helps reduce the wear and tear on the gums. Electric toothbrushes can be purchased for as little as $15 at the drugstore.
Proper oral hygiene is another way to prevent sensitive teeth. Most people only spend less than 45 seconds brushing their teeth, when in actuality it takes 2-3 minutes to thoroughly brush your teeth. Brushing your teeth quickly leaves some of the tooth structure unclean, which leads to plaque, then bacteria and ultimately gingivitis and receding gums.
Treating Sensitive Teeth
If you already have sensitive teeth, there is a treatment available. Potassium nitrate, which is found in sensitivity toothpastes, reduces tooth sensitivity. Sensodyne toothpaste is the #1 recommended toothpaste by dentists to treat sensitive teeth. Sensodyne is so effective that it begins to reduce tooth sensitivity within a few uses. When using Sensodyne, make sure that you are brushing properly and avoiding acidic foods to maximize its effectiveness.
When to see your dentist
If your sensitivity is so severe that switching to an electric brush and using sensitivity toothpaste does not work, then there is a treatment option available from your dentist. Your dentist can use oxalate compounds to treat the root, which will eliminate the sensitivity. There is also a bonding process available to seal the pores of the root.
If you have mild tooth sensitivity, there are toothpastes that are designed to protect the tubules. While it is an over the counter treatment, you should see your dentist to be sure that this is the right treatment. If the sensitivity is caused by another condition, your dentist can make a determination in one visit. In addition to the pain that tooth sensitivity causes, you can also develop inflammation that is not reversible. This condition can lead to an abscess that is only treated by oral surgery. Therefore, while tooth sensitivity starts out as a seemingly simple issue, it can lead to a serious condition. Your biannual checkups are the best time to discuss tooth sensitivity with your dentist. Your dentist can track the condition and visually inspect your teeth, which enables him to make the proper recommendations for your mouth.
Tuesday, June 11, 2013
Wisdom Teeth
Wisdom teeth are called
that because they appear during the adult years, when people are usually
considered ‘wiser’ than they were when their first set of teeth appeared as
children. Wisdom teeth are the third set of molars that come in during the late
teens and adulthood. Depending on your situation, wisdom teeth can be a blessing
or a curse.
If you have spaces between your teeth and room for them, wisdom teeth assist in naturally filling the gaps between your other teeth. This is usually not the case, however. For the majority of the population, wisdom teeth come in at an angle and there is not enough room to accommodate them in the mouth. Some wisdom teeth do not come in fully and cause infection and pain.
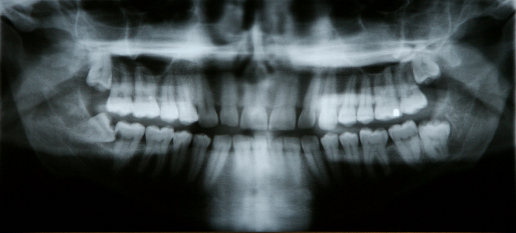
When your wisdom teeth come in, your dentist is the only one who can definitely say if they need to be removed. An exam, along with mouth x-rays, tell the full story about the growth of the wisdom teeth and if they need to be removed. As with other routine extractions, wisdom teeth are usually pulled. In some cases however, oral surgery is required to completely remove the tooth. Rather than taking a wait and see approach, it is recommended that you see your dentist at the first signs of the wisdom teeth. If you wait until they are a problem, damage to other healthy teeth can occur.
How are wisdom teeth removed?
Just as with any oral procedure, your dentist will numb the tooth and the surrounding area with a local anesthetic, similar to the type used when you have a cavity filled. The anesthetic will take care of the pain, but not any anxiety. The anxiety can easily be controlled with nitrous oxide or valium. Usually, you can drive yourself home after the nitrous oxide, but you will require a ride home if you choose valium. Once you are fully numb and relaxed, the dentist will proceed to pull the wisdom tooth.
What can I expect afterward?
After the wisdom tooth is removed, you will need some recovery time. The length of time necessary and extent of the after effects will depend on how easy the procedure was. If the wisdom tooth was fully erupted, then it will usually come out easily, with no complications. If the tooth is impacted, then it will require more work and damage to the surrounding gum tissue to remove. In general, the area will be completely healed within a few months. Usually you can resume your daily activities within 24 hours of the extraction. Your dentist will provide you with follow up care for your specific situation.
Are there any complications?
One common complication of wisdom tooth extraction is dry socket. Dry socket refers to a condition where the blood clot that forms in the tooth socket becomes dislodged. When this happens, the patient experiences moderate to severe pain in the site where the tooth was. The dentist can correct this condition with medication specifically designed to heal the tooth socket.
Another complication is called Paresthesia. This is a less frequently occurring complication. Paresthesia occurs when the nerves surrounding the tooth become damaged during the removal of an impacted wisdom tooth. The condition does not cause pain, but rather numbness of the chin, tongue, or lip. The numbness can last for a few weeks or become permanent.
If you have spaces between your teeth and room for them, wisdom teeth assist in naturally filling the gaps between your other teeth. This is usually not the case, however. For the majority of the population, wisdom teeth come in at an angle and there is not enough room to accommodate them in the mouth. Some wisdom teeth do not come in fully and cause infection and pain.
When your wisdom teeth come in, your dentist is the only one who can definitely say if they need to be removed. An exam, along with mouth x-rays, tell the full story about the growth of the wisdom teeth and if they need to be removed. As with other routine extractions, wisdom teeth are usually pulled. In some cases however, oral surgery is required to completely remove the tooth. Rather than taking a wait and see approach, it is recommended that you see your dentist at the first signs of the wisdom teeth. If you wait until they are a problem, damage to other healthy teeth can occur.
How are wisdom teeth removed?
Just as with any oral procedure, your dentist will numb the tooth and the surrounding area with a local anesthetic, similar to the type used when you have a cavity filled. The anesthetic will take care of the pain, but not any anxiety. The anxiety can easily be controlled with nitrous oxide or valium. Usually, you can drive yourself home after the nitrous oxide, but you will require a ride home if you choose valium. Once you are fully numb and relaxed, the dentist will proceed to pull the wisdom tooth.
What can I expect afterward?
After the wisdom tooth is removed, you will need some recovery time. The length of time necessary and extent of the after effects will depend on how easy the procedure was. If the wisdom tooth was fully erupted, then it will usually come out easily, with no complications. If the tooth is impacted, then it will require more work and damage to the surrounding gum tissue to remove. In general, the area will be completely healed within a few months. Usually you can resume your daily activities within 24 hours of the extraction. Your dentist will provide you with follow up care for your specific situation.
Are there any complications?
One common complication of wisdom tooth extraction is dry socket. Dry socket refers to a condition where the blood clot that forms in the tooth socket becomes dislodged. When this happens, the patient experiences moderate to severe pain in the site where the tooth was. The dentist can correct this condition with medication specifically designed to heal the tooth socket.
Another complication is called Paresthesia. This is a less frequently occurring complication. Paresthesia occurs when the nerves surrounding the tooth become damaged during the removal of an impacted wisdom tooth. The condition does not cause pain, but rather numbness of the chin, tongue, or lip. The numbness can last for a few weeks or become permanent.
Wisdom tooth removal is
a common procedure that has low risks associated with it. If you are uncertain
if your wisdom teeth need to be removed, contact your dentist and make an
appointment.
Friday, May 3, 2013
Dental Care Options During Trying Financial Times

The reality is that
many people who do not have dental insurance or the means to pay for services
will not visit the dentist. In these trying economic times hundreds of thousands
of people have lost their jobs and their dental insurance along with them. Even
those who are fortunate enough to still be employed view dental care as
something you get if you absolutely need it. Generally, dental services are
viewed by most as a response to an immediate dental condition, such as a cavity,
and not a preventative measure, such as mammograms and colon cancer
screening.
In the United States, dental care is expensive. Even those who are gainfully employed struggle with their dental co-payments. If they get a cavity it will only be fixed once they can save up the money to do it. Some of them will choose to pay $50 to pull a tooth with a small cavity, because filling the cavity costs $150.
There is also segment of the population who, despite the severity of the situation, cannot afford dental care. These are the people who cannot afford their rent or food for their family if they have to get a tooth pulled. There are literally millions of people who are in this category. They rely on home remedies and over the counter medication like pain killers to relieve the pain, but the pain never really goes away. There are many resources available at the local, state, and Federal level to assist.
This article has been written to examine the dental care options that are available to the general public.
Clinical Trials
Clinical trials are health related research studies using people. Clinical trials follow a strict protocol and are highly regulated by the Federal Government and the FDA. Every year, thousands of patients participate in clinical trials. Dental clinical trials have led to new technologies in fluoride treatments, safety findings, such as the use of mercury fillings, and new materials for prosthetic devices. Clinical trials take dental patients on a volunteer basis to test out new dental procedures. The benefits to the patient are that they gain free access to new dental treatments before they are available to the general public. All services are at no cost and, sometimes, the patient is compensated for their time. There are certain qualifying and exclusionary guidelines for patients seeking to be a part of each individual clinical trial. In general, dental clinical trials are extremely safe and a great benefit to both the patient and the community at large.
Dental School Clinics
Dental schools practice on real patients. The dental student or resident performs the procedures with a faculty member overseeing the work. The faculty member is a licensed dentist with a substantial amount of practical experience. They ensure that the patient is given quality care. The dental student will do a complete overview of your health and dental history and perform routine services such as x-rays. Most dental schools offer free and low cost services to the community. The only drawback to obtaining services at a dental school clinic is that the process of submitting an application to the school, being screened and then finally receiving treatment is a bit longer than obtaining services from a neighborhood dentist. If you are in need of emergency dental care, a dental school clinic will not be the most practical option for you.
Non Profit and Governmental agencies
The Centers for Medicare & Medicaid Services offer dental plans to low income families. The United Way also has referral services to low cost and no cost dentists in the local community. The service qualifications vary from agency to agency. Some have very liberal income requirements and others offer substantially reduced fees, with no qualifying necessary. Many of these agencies are overlooked by people because they assume that they will not qualify for services based on their income, employment, or citizenship status. This could not be farther from the truth. The agencies offering the care serve a broad spectrum of the community, not only a narrow scope of those who fit a certain profile.
It should be noted that, in response to the economic downturn, neighborhood dentists are now offering low cost financing options and some offer no cost payment plans.
If you need to see a dentist, do not put it off. A little research can uncover a wealth of resources and enable you to afford the care that you and your family need.
In the United States, dental care is expensive. Even those who are gainfully employed struggle with their dental co-payments. If they get a cavity it will only be fixed once they can save up the money to do it. Some of them will choose to pay $50 to pull a tooth with a small cavity, because filling the cavity costs $150.
There is also segment of the population who, despite the severity of the situation, cannot afford dental care. These are the people who cannot afford their rent or food for their family if they have to get a tooth pulled. There are literally millions of people who are in this category. They rely on home remedies and over the counter medication like pain killers to relieve the pain, but the pain never really goes away. There are many resources available at the local, state, and Federal level to assist.
This article has been written to examine the dental care options that are available to the general public.
Clinical Trials
Clinical trials are health related research studies using people. Clinical trials follow a strict protocol and are highly regulated by the Federal Government and the FDA. Every year, thousands of patients participate in clinical trials. Dental clinical trials have led to new technologies in fluoride treatments, safety findings, such as the use of mercury fillings, and new materials for prosthetic devices. Clinical trials take dental patients on a volunteer basis to test out new dental procedures. The benefits to the patient are that they gain free access to new dental treatments before they are available to the general public. All services are at no cost and, sometimes, the patient is compensated for their time. There are certain qualifying and exclusionary guidelines for patients seeking to be a part of each individual clinical trial. In general, dental clinical trials are extremely safe and a great benefit to both the patient and the community at large.
Dental School Clinics
Dental schools practice on real patients. The dental student or resident performs the procedures with a faculty member overseeing the work. The faculty member is a licensed dentist with a substantial amount of practical experience. They ensure that the patient is given quality care. The dental student will do a complete overview of your health and dental history and perform routine services such as x-rays. Most dental schools offer free and low cost services to the community. The only drawback to obtaining services at a dental school clinic is that the process of submitting an application to the school, being screened and then finally receiving treatment is a bit longer than obtaining services from a neighborhood dentist. If you are in need of emergency dental care, a dental school clinic will not be the most practical option for you.
Non Profit and Governmental agencies
The Centers for Medicare & Medicaid Services offer dental plans to low income families. The United Way also has referral services to low cost and no cost dentists in the local community. The service qualifications vary from agency to agency. Some have very liberal income requirements and others offer substantially reduced fees, with no qualifying necessary. Many of these agencies are overlooked by people because they assume that they will not qualify for services based on their income, employment, or citizenship status. This could not be farther from the truth. The agencies offering the care serve a broad spectrum of the community, not only a narrow scope of those who fit a certain profile.
It should be noted that, in response to the economic downturn, neighborhood dentists are now offering low cost financing options and some offer no cost payment plans.
If you need to see a dentist, do not put it off. A little research can uncover a wealth of resources and enable you to afford the care that you and your family need.
Wednesday, March 6, 2013
Special Needs Patients

People with special
needs need dental treatment as much as those without special needs, yet they
receive dental care less frequently. Special needs patients may have a mental or
physical disability or have a chronic physical condition. There are community
based dental programs which specifically aim to improve the dental health of
special needs patients. If your community does not have any of these programs,
any dentist is qualified to provide the care necessary for dental health. The
most common special needs identified by the dental community are patients with
immunocompromised disorders, autism, and Down ’s syndrome.
Immunocompromised patients and dental treatment
One challenge for the dental community is patients with immunocompromised disorders. Patients with immunocompromised disorders have issues that tend to be caused by tobacco use, malnutrition, and poor oral hygiene. Patients with leukaemia develop gingival bleeding and purpura. Patients with herpes viral infections develop lesions, ulcers, and periodontal disease. Patients with a low white cell count development oral lesions. This condition is controlled by antiretroviral medication. The dentist should be made aware of all conditions that an immunocompromised patient is afflicted with. The dentist will then take whatever special precautions are necessary to administer the dental services, while protecting the patient’s immune system.
Mentally challenged patients with poor oral health increase their struggle for social acceptance by allowing their teeth to deteriorate. Challenges to treating mentally ill patients include fear and lack of training on the part of dental professionals. Patients with Down’s syndrome and Autism are in the same situation.
Down’s syndrome and Dental treatment
Patients with Down’s syndrome many times have significant impairments of the mouth. Children who are afflicted with Down’s syndrome experience delayed development of the teeth and jaw. Sometimes the first tooth will not erupt until after the first 18 months and the complete set of teeth may not all appear until after three years of age. This, in turn, delays the adult teeth. It is not uncommon for Down’s syndrome patients to be missing adult teeth and many times the teeth are smaller than that of a patient without Down’s syndrome.
Patients with Down’s syndrome require a different approach to a routine dental appointment. The dentist and staff need additional time to explain the procedure and possibly move at a slower pace during the visit to allow the patient to develop a level of comfort. With Down’s syndrome adults and children, it is recommended that the procedure be demonstrated and then the patient be allowed to ask questions and express any concerns. Down’s syndrome patients have a larger and thicker tongue than other patients, which makes it a logistical challenge to accommodate the tongue during cleanings and examinations. In addition, patients with Down’s syndrome have reduced muscle tone in the mouth. This results in less rigorous chewing and additional food particles left in the mouth and on the teeth after eating. For the dentist, this means that cleanings may need to be scheduled more frequently and the patient should be educated on merits of brushing after every meal. The dentist would also want to take additional time to demonstrate the use of an electric toothbrush and floss holders.
Autism and dental treatment
Autism is a neurological disorder that emerges during the first three years of a child’s life. The syndrome affects the areas of the brain that are responsible for social interaction skills and communication. Delayed and reduced social skills, interactive speech limitations, and sensorimotor defects are the main symptoms of Autism. Children with Autism look just like any other child, but they experience challenges functioning and communicating in a social environment. Patients with Autism should be slowly introduced to the dental environment. Autistic patients will be comforted by bringing a familiar item with them for comfort such as a blanket or favorite toy. The caregiver is the best person to guide the dentist on the best method of approach, which would cause the patient the least amount of stress and anxiety in the situation. The dental staff should meet with the caregiver prior to the treatment to ensure that the patient is in a setting that they are comfortable with.
If you or a loved one has special needs, it is important to seek regular dental treatment. It is recommended that prior to making an appointment that you discuss the special needs with the receptionist and ask if their office can accommodate you. If their response is favorable, make an appointment to interview the dentist. Discuss with the dentist the full scope of the patient’s medical condition and what special needs he/she has. Ask the dentist if he treats other patients with special needs and what special training he has to address your specific needs. More often than not, this interview will allow the dentist to develop a treatment plan for the patient. Dentists are doctors committed to oral health. Most diseases and conditions have an effect upon the mouth, teeth, and gums and dentists understand the broad scope of treatments required.
Immunocompromised patients and dental treatment
One challenge for the dental community is patients with immunocompromised disorders. Patients with immunocompromised disorders have issues that tend to be caused by tobacco use, malnutrition, and poor oral hygiene. Patients with leukaemia develop gingival bleeding and purpura. Patients with herpes viral infections develop lesions, ulcers, and periodontal disease. Patients with a low white cell count development oral lesions. This condition is controlled by antiretroviral medication. The dentist should be made aware of all conditions that an immunocompromised patient is afflicted with. The dentist will then take whatever special precautions are necessary to administer the dental services, while protecting the patient’s immune system.
Mentally challenged patients with poor oral health increase their struggle for social acceptance by allowing their teeth to deteriorate. Challenges to treating mentally ill patients include fear and lack of training on the part of dental professionals. Patients with Down’s syndrome and Autism are in the same situation.
Down’s syndrome and Dental treatment
Patients with Down’s syndrome many times have significant impairments of the mouth. Children who are afflicted with Down’s syndrome experience delayed development of the teeth and jaw. Sometimes the first tooth will not erupt until after the first 18 months and the complete set of teeth may not all appear until after three years of age. This, in turn, delays the adult teeth. It is not uncommon for Down’s syndrome patients to be missing adult teeth and many times the teeth are smaller than that of a patient without Down’s syndrome.
Patients with Down’s syndrome require a different approach to a routine dental appointment. The dentist and staff need additional time to explain the procedure and possibly move at a slower pace during the visit to allow the patient to develop a level of comfort. With Down’s syndrome adults and children, it is recommended that the procedure be demonstrated and then the patient be allowed to ask questions and express any concerns. Down’s syndrome patients have a larger and thicker tongue than other patients, which makes it a logistical challenge to accommodate the tongue during cleanings and examinations. In addition, patients with Down’s syndrome have reduced muscle tone in the mouth. This results in less rigorous chewing and additional food particles left in the mouth and on the teeth after eating. For the dentist, this means that cleanings may need to be scheduled more frequently and the patient should be educated on merits of brushing after every meal. The dentist would also want to take additional time to demonstrate the use of an electric toothbrush and floss holders.
Autism and dental treatment
Autism is a neurological disorder that emerges during the first three years of a child’s life. The syndrome affects the areas of the brain that are responsible for social interaction skills and communication. Delayed and reduced social skills, interactive speech limitations, and sensorimotor defects are the main symptoms of Autism. Children with Autism look just like any other child, but they experience challenges functioning and communicating in a social environment. Patients with Autism should be slowly introduced to the dental environment. Autistic patients will be comforted by bringing a familiar item with them for comfort such as a blanket or favorite toy. The caregiver is the best person to guide the dentist on the best method of approach, which would cause the patient the least amount of stress and anxiety in the situation. The dental staff should meet with the caregiver prior to the treatment to ensure that the patient is in a setting that they are comfortable with.
If you or a loved one has special needs, it is important to seek regular dental treatment. It is recommended that prior to making an appointment that you discuss the special needs with the receptionist and ask if their office can accommodate you. If their response is favorable, make an appointment to interview the dentist. Discuss with the dentist the full scope of the patient’s medical condition and what special needs he/she has. Ask the dentist if he treats other patients with special needs and what special training he has to address your specific needs. More often than not, this interview will allow the dentist to develop a treatment plan for the patient. Dentists are doctors committed to oral health. Most diseases and conditions have an effect upon the mouth, teeth, and gums and dentists understand the broad scope of treatments required.
Friday, February 1, 2013
Pregnancy and your teeth
Pregnancy is a special time for couples. It is filled with excitement for the mother to be. Pregnancy can also be a stressful time as pregnancy brings with it the risk of complications like high blood pressure, gestational diabetes, and hypertension. One complication that most pregnant women do not consider is dental complications. If not treated, dental complications can complicate the pregnancy instead of only being a byproduct of the pregnancy. Some of the dental problems that pregnant women are likely to experience are pregnancy gingivitis, pregnancy tumors, and periodontal disease.
While you are pregnant, you should adjust your dental routine and be on the lookout for different indications of a dental issue. It is recommended that you have at least two checkups during your pregnancy; one for a cleaning and the other for a checkup. The optimal time to make the appointments is after the first trimester, as this is after your baby has formed its vital organs. Cleanings are not detrimental during any time during the pregnancy but, to be extra careful, waiting until the second trimester is best.
If you have any tooth pain or notice changes in your gum line during your pregnancy, you should see your dentist immediately. These symptoms are signs of infection. Any infection, no matter how small, puts your body and baby at risk.
Pregnancy gingivitis
Almost 60% of all pregnant women experience gingivitis during their pregnancy. Pregnancy gingivitis causes inflamed and red gums. It also causes bleeding during routine brushing and flossing. This is caused by bacteria between your teeth which cause the gums to become inflamed. Pregnant women are at high risk because of the increased levels of progesterone and estrogen in their bodies. The risk for gum disease increases in the second and third trimester. The best way to prevent pregnancy gingivitis is to continue with a good oral hygiene regimen during your pregnancy. During pregnancy, women find it difficult to keep up with regular doctor visits, let alone go to the dentist. This is a mistake as both are equally important to the baby’s and mother’s health.
Pregnancy tumors
A pregnancy tumor is a growth that spontaneously occurs in the mouth during the second trimester. Pregnancy tumors are not cancerous and range in size from quite small to large enough to disrupt regular activities. Pregnancy tumors, appearing as a red or purple bump, can occur anywhere in the mouth. Upon closer inspection, the bump is attached to the gum tissue by a thin stem of skin. The tumor will bleed easily and many times will turn into an open sore. While the tumor itself is not dangerous, the appearance can cause alarm. The dentist removes the tumor during a simple office procedure called a biopsy. The tissue is removed and then examined in a laboratory to ensure that it is benign. Once the woman gives birth, the tumors will become smaller and eventually disappear altogether. Pregnancy tumors can be prevented by having regular cleanings while pregnant. In some instances, however, there is no prevention because higher levels of hormones cause the growth.
Periodontal disease
Periodontal disease is an advanced form of gingivitis. Unlike gingivitis, periodontal disease affects the gums and jawbone. Periodontal disease is so severe that many times it requires surgical procedures to remove the decayed gums and restore the gum line. As with other pregnancy conditions of the mouth, frequent brushing, flossing and regular cleanings are key to preventing the disease.
If you are pregnant, add a dental exam to your medical schedule by the second trimester. Just as ultrasounds and other exams are vital to a healthy pregnancy, so is a trip to your dentist.
While you are pregnant, you should adjust your dental routine and be on the lookout for different indications of a dental issue. It is recommended that you have at least two checkups during your pregnancy; one for a cleaning and the other for a checkup. The optimal time to make the appointments is after the first trimester, as this is after your baby has formed its vital organs. Cleanings are not detrimental during any time during the pregnancy but, to be extra careful, waiting until the second trimester is best.
If you have any tooth pain or notice changes in your gum line during your pregnancy, you should see your dentist immediately. These symptoms are signs of infection. Any infection, no matter how small, puts your body and baby at risk.
Pregnancy gingivitis
Almost 60% of all pregnant women experience gingivitis during their pregnancy. Pregnancy gingivitis causes inflamed and red gums. It also causes bleeding during routine brushing and flossing. This is caused by bacteria between your teeth which cause the gums to become inflamed. Pregnant women are at high risk because of the increased levels of progesterone and estrogen in their bodies. The risk for gum disease increases in the second and third trimester. The best way to prevent pregnancy gingivitis is to continue with a good oral hygiene regimen during your pregnancy. During pregnancy, women find it difficult to keep up with regular doctor visits, let alone go to the dentist. This is a mistake as both are equally important to the baby’s and mother’s health.
Pregnancy tumors
A pregnancy tumor is a growth that spontaneously occurs in the mouth during the second trimester. Pregnancy tumors are not cancerous and range in size from quite small to large enough to disrupt regular activities. Pregnancy tumors, appearing as a red or purple bump, can occur anywhere in the mouth. Upon closer inspection, the bump is attached to the gum tissue by a thin stem of skin. The tumor will bleed easily and many times will turn into an open sore. While the tumor itself is not dangerous, the appearance can cause alarm. The dentist removes the tumor during a simple office procedure called a biopsy. The tissue is removed and then examined in a laboratory to ensure that it is benign. Once the woman gives birth, the tumors will become smaller and eventually disappear altogether. Pregnancy tumors can be prevented by having regular cleanings while pregnant. In some instances, however, there is no prevention because higher levels of hormones cause the growth.
Periodontal disease
Periodontal disease is an advanced form of gingivitis. Unlike gingivitis, periodontal disease affects the gums and jawbone. Periodontal disease is so severe that many times it requires surgical procedures to remove the decayed gums and restore the gum line. As with other pregnancy conditions of the mouth, frequent brushing, flossing and regular cleanings are key to preventing the disease.
If you are pregnant, add a dental exam to your medical schedule by the second trimester. Just as ultrasounds and other exams are vital to a healthy pregnancy, so is a trip to your dentist.
Friday, January 11, 2013
Diabetes and Oral Health
According to the American Dental Association, 21 million Americans have diabetes. Diabetes is a disease that affects the entire body. People with diabetes have a greater risk for health problems because they are unable to control their blood sugar levels. Uncontrolled blood sugar disables the white blood cells’ ability to fight infection. White blood cells are the body’s key defense to infection. Without them working at full capacity, you are at greater risk for infections of the mouth. People with diabetes who smoke are 10 times higher to develop the following conditions because smoking hinders the blood flow to the gums, which interferes with healing.
Conditions commonly associated with diabetes:
Dry Mouth – Low blood sugar decreases saliva flow and leads to dry mouth. The condition leads to sores, ulcers, and infections.
Gum Inflammation/Periodontal Disease – Aside from the other complications of diabetes, these people have a high risk for developing an advanced form of gum disease called periodontitis. Diabetes patients can reduce their risk of periodontitis by controlling their blood sugar levels. The mere presence of periodontitis will make your blood sugar harder to control as the disease causes infection in the body.
Diabetes impairs white blood cells, which thickens blood vessels, and ultimately slows down the flow of nutrients and other materials through the body. This causes infection and periodontal disease. Periodontal disease is a bacterial infection, and since diabetics are less able to fight infection, they will experience a more severe periodontal disease than non diabetics.
Periodontitis causes your gums to pull away from your teeth. When this happens, pockets form between your teeth and gums. These pockets trap bacteria and germs, which eventually turn into puss. The more material that is in the crevices, the bigger they get. The only way to reverse periodontitis is oral surgery. If the condition is not treated, the teeth will decay to the point of requiring extraction and the remaining teeth will shift. In advanced cases of periodontitis, teeth have been known to simply fall out.
Slow or poor healing in the mouth – People with diabetes, in general, heal slowly. This is due to the impaired blood flow that uncontrolled blood sugars causes. Even a simple cavity can be a major event for a diabetic.
Thrush – Diabetics are prone to fungal infections. One such fungal infection is called Thrush. It develops in the mouth and tongue. Thrush thrives on the high sugar levels in the saliva when diabetes is uncontrolled. Thrush also produces a burning sensation in the mouth and the tongue.
The best way for diabetes patients to prevent these conditions is to control your blood sugar levels. There is a direct link between high glucose levels and oral disease. Develop healthy oral habits such as brushing regularly, flossing, and dental checkups twice per year. Don’t smoke. While smoking is not good for anyone, diabetes patients are several times as likely to develop smoking related conditions than non diabetic patients.
Dental care and diabetes –It is imperative that diabetics stick to a good oral healthcare routine because they are at a higher risk for the diseases mentioned above. The first habit is to never miss a checkup visit. When identified early, infections and conditions of the mouth can be treated before they become a serious problem. At each visit, update your dentist on your diabetes condition and blood sugar levels. Share your diabetes doctor’s contact information prior to any oral procedures. Brush with a soft bristled toothbrush, floss regularly and have your teeth cleaned twice per year.
Common questions and myths about diabetes:
Does diabetes increase the risk of cavities?
The answer is yes and no. People with diabetes that control their blood sugar levels and have good oral hygiene are not at greater risk for cavities. When diabetics do not control their blood sugar levels, bacteria that cause cavities increases and the result is more cavities. In addition, since diabetics typically eat more meals throughout the day to control their blood sugar, they need to brush their teeth more frequently. In contrast, diabetics refrain from eating high sugar foods, which would put them at a lower risk than a non-diabetic person who eats those foods. As long as the disease is under control, the risk is mitigated.
Are diabetics at higher risk for complications when undergoing oral surgery?
Diabetics are at greater risk when undergoing any surgical procedure because they heal slower and are at greater risk for infection. This risk is managed by administering antibiotics prior to the surgery and additional follow up visits after surgery to monitor the healing process. If the patient smokes, they must not smoke two weeks before and at least two weeks after oral surgery. Smoking increases the risk of infection in a non-diabetic patient. For diabetics, smoking increases the chance of infection ten times that of a non- diabetic person.
If you are diabetic, speak with your dentist about preventative measures that will ensure your oral health. Taking a proactive approach will save your teeth in the long run. The less damage you do to your teeth, the better off you will be down the road. You have only one set of teeth; treat them right!
Conditions commonly associated with diabetes:
Dry Mouth – Low blood sugar decreases saliva flow and leads to dry mouth. The condition leads to sores, ulcers, and infections.
Gum Inflammation/Periodontal Disease – Aside from the other complications of diabetes, these people have a high risk for developing an advanced form of gum disease called periodontitis. Diabetes patients can reduce their risk of periodontitis by controlling their blood sugar levels. The mere presence of periodontitis will make your blood sugar harder to control as the disease causes infection in the body.
Diabetes impairs white blood cells, which thickens blood vessels, and ultimately slows down the flow of nutrients and other materials through the body. This causes infection and periodontal disease. Periodontal disease is a bacterial infection, and since diabetics are less able to fight infection, they will experience a more severe periodontal disease than non diabetics.
Periodontitis causes your gums to pull away from your teeth. When this happens, pockets form between your teeth and gums. These pockets trap bacteria and germs, which eventually turn into puss. The more material that is in the crevices, the bigger they get. The only way to reverse periodontitis is oral surgery. If the condition is not treated, the teeth will decay to the point of requiring extraction and the remaining teeth will shift. In advanced cases of periodontitis, teeth have been known to simply fall out.
Slow or poor healing in the mouth – People with diabetes, in general, heal slowly. This is due to the impaired blood flow that uncontrolled blood sugars causes. Even a simple cavity can be a major event for a diabetic.
Thrush – Diabetics are prone to fungal infections. One such fungal infection is called Thrush. It develops in the mouth and tongue. Thrush thrives on the high sugar levels in the saliva when diabetes is uncontrolled. Thrush also produces a burning sensation in the mouth and the tongue.
The best way for diabetes patients to prevent these conditions is to control your blood sugar levels. There is a direct link between high glucose levels and oral disease. Develop healthy oral habits such as brushing regularly, flossing, and dental checkups twice per year. Don’t smoke. While smoking is not good for anyone, diabetes patients are several times as likely to develop smoking related conditions than non diabetic patients.
Dental care and diabetes –It is imperative that diabetics stick to a good oral healthcare routine because they are at a higher risk for the diseases mentioned above. The first habit is to never miss a checkup visit. When identified early, infections and conditions of the mouth can be treated before they become a serious problem. At each visit, update your dentist on your diabetes condition and blood sugar levels. Share your diabetes doctor’s contact information prior to any oral procedures. Brush with a soft bristled toothbrush, floss regularly and have your teeth cleaned twice per year.
Common questions and myths about diabetes:
Does diabetes increase the risk of cavities?
The answer is yes and no. People with diabetes that control their blood sugar levels and have good oral hygiene are not at greater risk for cavities. When diabetics do not control their blood sugar levels, bacteria that cause cavities increases and the result is more cavities. In addition, since diabetics typically eat more meals throughout the day to control their blood sugar, they need to brush their teeth more frequently. In contrast, diabetics refrain from eating high sugar foods, which would put them at a lower risk than a non-diabetic person who eats those foods. As long as the disease is under control, the risk is mitigated.
Are diabetics at higher risk for complications when undergoing oral surgery?
Diabetics are at greater risk when undergoing any surgical procedure because they heal slower and are at greater risk for infection. This risk is managed by administering antibiotics prior to the surgery and additional follow up visits after surgery to monitor the healing process. If the patient smokes, they must not smoke two weeks before and at least two weeks after oral surgery. Smoking increases the risk of infection in a non-diabetic patient. For diabetics, smoking increases the chance of infection ten times that of a non- diabetic person.
If you are diabetic, speak with your dentist about preventative measures that will ensure your oral health. Taking a proactive approach will save your teeth in the long run. The less damage you do to your teeth, the better off you will be down the road. You have only one set of teeth; treat them right!
Subscribe to:
Posts (Atom)